Lysyl oxidase inhibitors for haematoligical malignancies and solid tumours
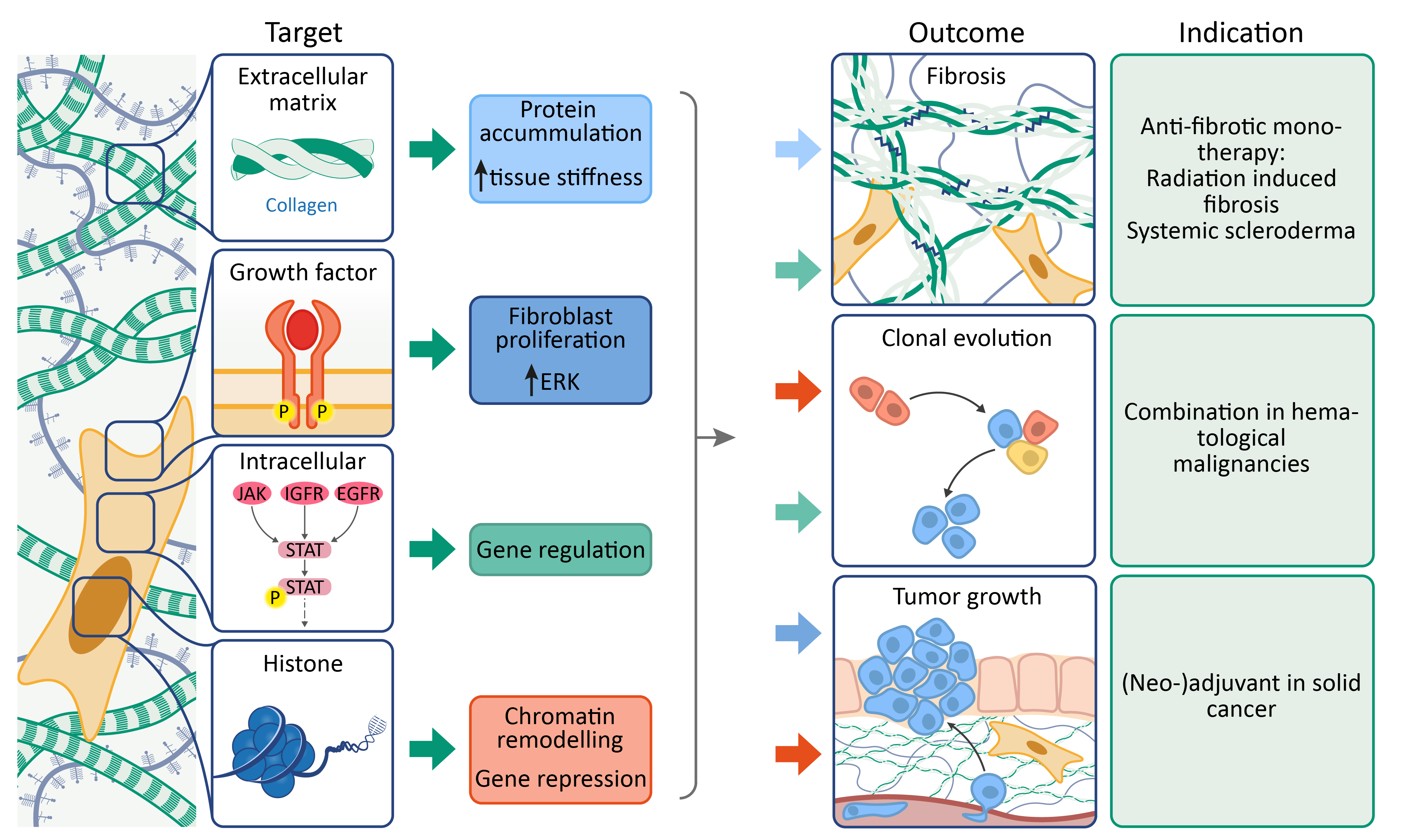
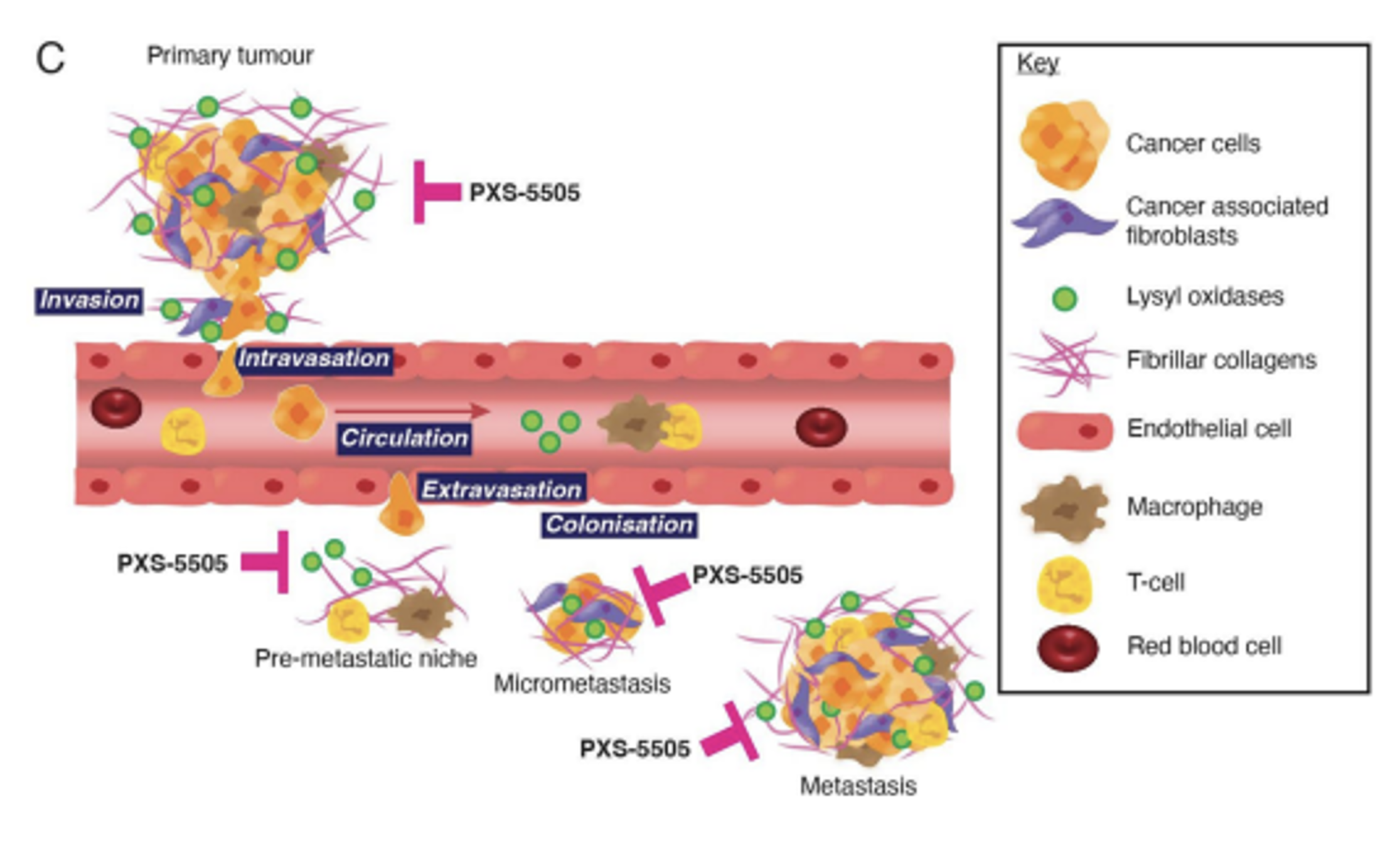
Lysyl oxidases are a family of five enzymes (LOXL and LOXL1-4) responsible for catalysing the formation of cross-links in collagen and elastin. In diseases states, excessive cross-link formation overwhelms endogenous degradation processes, shifting the balance towards hardened fibrotic tissue. This can occur in organs as well as the microenvironment surrounding tumours. The anti-fibrotic effects of lysyl oxidase inhibitors have been described in many diseases.
In addition to mediating collagen cross-link formation, lysyl oxidases also regulate growth factors. Inhibition of lysyl oxidases reduces the activation of platelet-derived growth factor receptors, further slowing fibrosis.
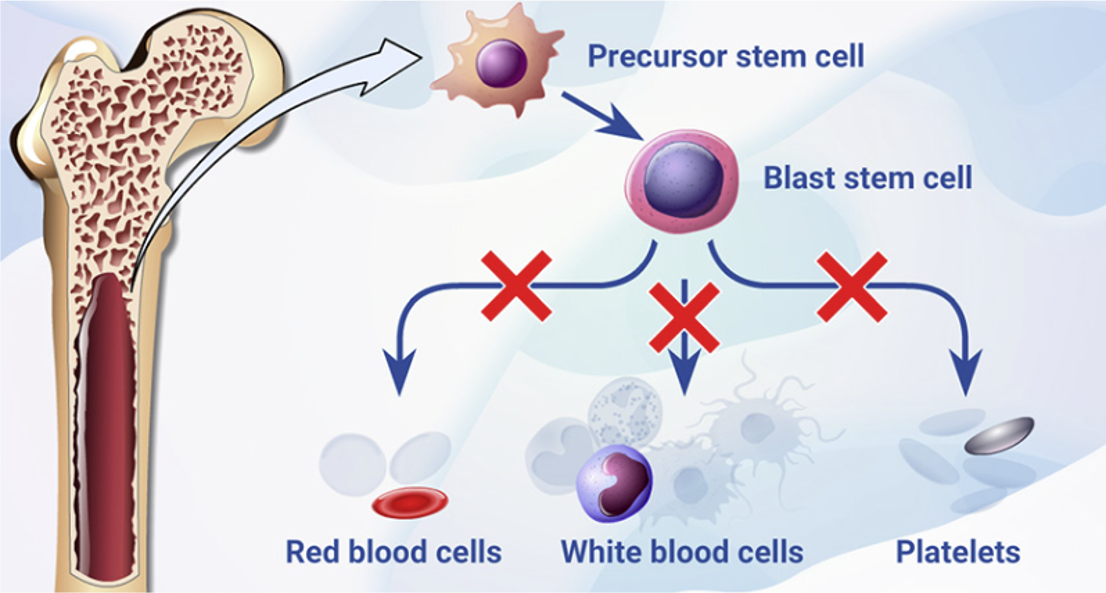
Besides these extra-nuclear effector functions, intra-cellular and intra-nuclear effects are also mediated by LOX, including gene regulation via the STAT pathway and histone modification. These effects, namely changing gene expression and promoting clonal selection, are implicated in haematological malignancies and solid tumours.